In questo articolo potete reperire tutte le informazioni relative all’uretroplastica per la stenosi dell’uretra bulbare distale:
- Uretroplastica bulbare in tempo unico con innesto VENTRALE di mucosa buccale
- Uretroplastica bulbare in tempo unico con innesto DORSALE di mucosa buccale
- Uretroplastica bulbare in tempo unico con innesto DORSALE di prepuzio
- Uretroplastica bulbare in tempo unico con innesto DORSALE + VENTRALE di mucosa buccale
- Uretroplastica bulbare in tempo unico con innesto DORSALE + VENTRALE di mucosa buccale e prepuzio
Uretroplastica bulbare in tempo unico con innesto VENTRALE di mucosa buccale
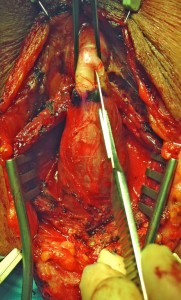
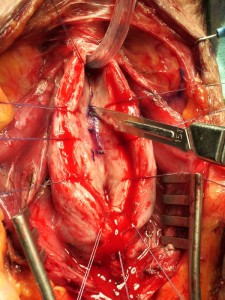
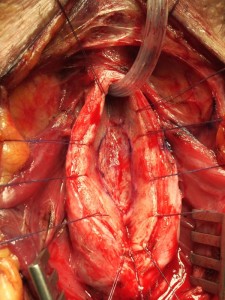
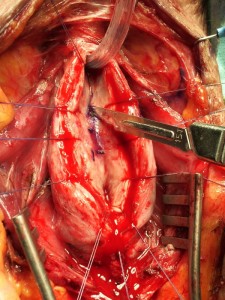
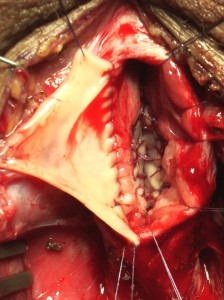
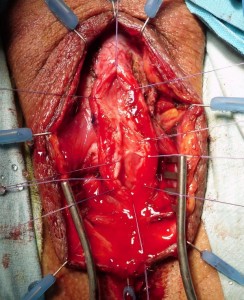
TECNICA: Incisione perineale ad Y rovesciata. Isolamento dell’uretra bulbare distale senza la sezione del centro tendineo del perineo. Apertura mediana ventrale dell’uretra, lungo il tratto stenotico [foto V1, V2]. Asportazione parziale di tessuto uretrale cicatriziale ed ampliamento del letto uretrale mediante innesto ventrale (sec. McAninch) di mucosa buccale (prelevata dalla guancia destra o sinistra) [foto V3, V4, V5]. Spongioplastica mediante sutura continua [foto V6]. Drenaggio. Parete a strati. Si consiglia Catetere Foley 18 Fr (siliconato e scanalato) per 21 giorni (sempre collegato al sacchetto della raccolta urine). Medicazione compressiva.
TEMPO DI ESECUZIONE: Circa 1,5h
TERAPIA: terapia antibiotica mirata in caso di urinocoltura positiva; antibioticoprofilassi con cefalosporina di III generazione in caso di uricocoltura negativa
GESTIONE PAZIENTE: il paziente deve rimanere a letto per 2 giorni con ghiaccio sul perineo. Ghiaccio sulla guancia per 1 giorno. Dimissioni in 3° giornata postoperatoria.
MEDICAZIONI: La ferita perineale può essere pulita con acqua. Tra catetere e meato escono delle secrezioni-incrostazioni che vanno pulite più volte al giorno. Si consiglia di utilizzare acqua o soluzione fisiologica su una garza per pulire il catetere.
URETROCISTOGRAFIA MINZIONALE: Importante effettuare l’uretrocistografia minzionale di controllo, a 21 giorni dall’intervento chirurgico,per verificare se ci sono fistole. La percentuale di fistola uretrale insorta dopo uretroplastica bulbare, effettuate nel nostro Centro, è il 5%. Tutte le fistole uretrali sono state risolte mediante il posizionamento di catetere uretrale per ulteriori 10 o 15 o 20 giorni, a seconda dell’entità della fistola.
QUANDO IMPIEGARE QUESTO TIPO DI URETROPLASTICA: stenosi bulbare corta (< 2cm) o lunga (> 2cm), ma solo se la stenosi non è obliterativa. Quando si apre l’uretra, se il piatto uretrale dorsale non è molto compromesso, è possibile effettuare un innesto ventrale con graft di mucosa buccale. Può essere indicata nei casi di lichen sclerosus dell’uretra e dei genitali, nonchè nei casi di ipospadia fallita (pazienti plurioperati per ipospadia) e nella ipospadia vergine.
COMPLICANZE: sanguinamento <1%, infezione <2%. Fistola 3%
PERCENTUALE DI SUCCESSO CENTRO URETRA AREZZO: Casistica aggiornata al 30/06/2015. Effettuate 768 uretroplastiche bulbari in tempo unico con mucosa buccale. Percentuale di successo 91.2%.
CENTRO URETRA IN ITALIA: èpossibile effetuare una Visita con il Dr. Palminteri o la Dr.ssa Berdondini presso una delle principali sedi: Arezzo, Torino, Milano, Modena, Roma, Napoli, Reggio Calabria, Bari, Brindisi, Palermo, Catania, Messina, Trapani.
APPROFONDIMENTI:
Long-term followup of the ventrally placed buccal mucosa onlay graft in bulbar urethral reconstruction. (Elliott SP, Metro MJ, McAninch JW.) J Urol. 2003 May;169(5):1754-7.
PURPOSE:We investigate whether the short-term success rate (greater than 90%) of buccal mucosa free grafts in the bulbar urethra is sustained in the long term. MATERIALS AND METHODS: In 60 patients a ventrally placed buccal mucosa graft was used for repair of bulbar urethral strictures. Of these patients 49 had undergone previous attempt at repair (urethroplasty in 4, internal urethrotomy in 45). Mean graft length was 4.8 cm. In 9 patients a distal penile fasciocutaneous flap was also used for repair of concomitant penile urethral stricture. In 8 of the 9 patients the buccal mucosa graft was combined with end-to-end urethroplasty and 2 buccal mucosa grafts were used in tandem in 1. Followup was at least 1 year in all cases (mean 47 months, range 12 to 107). Failure was defined as an obstructive voiding pattern with radiographic or cystoscopic evidence of recurrent stricture. RESULTS: Bulbar stricture repair was successful in 54 patients (90%) and 4 of the remaining 6 responded to 1 internal urethrotomy for a long-term success rate of 97%. Preoperative clinical characteristics were not significantly different between those who experienced success or failure. CONCLUSIONS: Long-term outcome analysis of ventrally placed buccal mucosa onlay grafts for bulbar urethral strictures demonstrates a durable success rate of 90%. This rate can be improved (97%) with the judicious use of internal urethrotomy.
A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. (Mangera A, Patterson JM, Chapple CR.) Eur Urol. 2011 May;59(5):797-814. Epub 2011 Feb 24. Review.
CONTEXT: Reconstructive surgeons who perform urethroplasty have a variety of techniques in their armamentarium that may be used according to factors such as aetiology, stricture position, and length. No one technique is recommended. OBJECTIVE: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. EVIDENCE ACQUISITION: We performed an updated systematic review of the Medline literature from 1985 to date and classified the data according to the site of surgery and technique used. Data are also presented on the type of graft used and the follow-up methodology used by each centre. EVIDENCE SYNTHESIS: More than 2000 anterior urethroplasty procedures have been described in the literature. When considering the bulbar urethra there is no significant difference between the average success rates of the dorsal and the ventral onlay procedures, 88.4% and 88.8% at 42.2 and 34.4 mo in 934 and 563 patients, respectively. The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. When considering penile strictures, the success rate of the two-stage penile technique is significantly better than the one-stage penile technique, 90.5% versus 75.7% as calculated for 129 and 432 patients, respectively, although the follow-up of one-stage procedures was longer at 32.8 mo compared with 22.2 mo. CONCLUSIONS: There is no evidence in the literature of a difference between one-stage techniques for urethroplasty of the bulbar urethra. The two-stage technique has better reported outcomes than a one-stage approach for penile urethroplasty but has a shorter follow-up.
Uretroplastica bulbare in tempo unico con innesto DORSALE di mucosa buccale
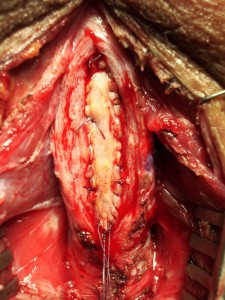
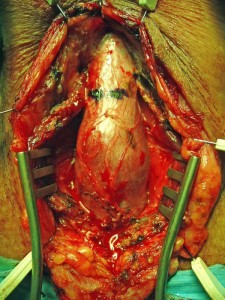
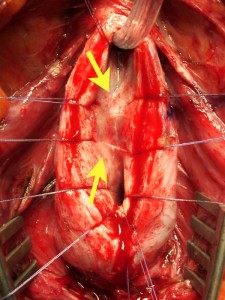
TECNICA: Incisione perineale ad Y rovesciata. Isolamento dell’uretra bulbare distale senza la sezione del centro tendineo del perineo. Apertura mediana ventrale dell’uretra, lungo il tratto stenotico [foto A1, A2]. Incisione mediana del piatto uretrale stenotico e lateralizzazione delle due bande di spongiosa [foto A3, A4]. Asportazione parziale del tessuto cicatriziale uretrale a livello della stenosi. Si confeziona uretroplastica di ampliamento dorsale (sec. Asopa) con innesto di mucosa buccale (prelevata dalla guancia destra o sinistra) [foto A5,A6]. Spongioplastica mediante sutura continua [foto A7]. Drenaggio. Parete a strati. Si consiglia Catetere Foley 18 Fr (siliconato e scanalato) per 21 giorni (sempre collegato al sacchetto della raccolta urine). Medicazione compressiva.
TEMPO DI ESECUZIONE: Circa 1,5h
TERAPIA: terapia antibiotica mirata in caso di urinocoltura positiva; antibioticoprofilassi con cefalosporina di III generazione in caso di uricocoltura negativa.
GESTIONE PAZIENTE: il paziente deve rimanere a letto per 2 giorni con ghiaccio sul perineo. Ghiaccio sulla guancia per 1 giorno. Dimisisoni in 3° giornata postoperatoria.
MEDICAZIONI: La ferita perineale può essere pulita con acqua. Tra catetere e meato escono delle secrezioni-incrostazioni che vanno pulite più volte al giorno. Si consiglia di utilizzare acqua o soluzione fisiologica su una garza per pulire il catetere.
URETROCISTOGRAFIA MINZIONALE: Importante effettuare l’uretrocistografia minzionale di controllo, a 21 giorni dall’intervento chirurgico,per verificare se ci sono fistole. La percentuale di fistola uretrale insorta dopo uretroplastica bulbare, effettuate nel nostro Centro, è il 5%. Tutte le fistole uretrali sono state risolte mediante il posizionamento di catetere uretrale per ulteriori 10 o 15 o 20 giorni, a seconda dell’entità della fistola.
QUANDO IMPIEGARE QUESTO TIPO DI URETROPLASTICA: stenosi bulbare corta (< 2cm) o lunga (> 2cm), ma solo se la stenosi non è obliterativa. Quando si apre l’uretra, se il piatto uretrale è molto compromesso dorsalmente, viene parzialmente asportato e sostituito con la mucosa buccale. Può essere indicata nei casi di lichen sclerosus dell’uretra e dei genitali, nonchè nei casi di ipospadia fallita (pazienti plurioperati per ipospadia) e nella ipospadia vergine.
COMPLICANZE: sanguinamento <1%, infezione <2%. Fistola 4%
PERCENTUALE DI SUCCESSO CENTRO URETRA AREZZO: Casistica aggiornata al 30/06/2015. Effettuate 75 uretroplastiche bulbari in tempo unico con mucosa buccale. Percentuale di successo 89.4%.
CENTRO URETRA IN ITALIA: èpossibile effetuare una Visita con il Dr. Palminteri o la Dr.ssa Berdondini presso una delle principali sedi: Arezzo, Torino, Milano, Modena, Roma, Napoli, Reggio Calabria, Bari, Brindisi, Palermo, Catania, Messina, Trapani.
APPROFONDIMENTI:
Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. (Asopa HS, Garg M, Singhal GG, Singh L, Asopa J, Nischal A.) Urology. 2001 Nov;58(5):657-9.
OBJECTIVES: To explore the feasibility of applying a dorsal free graft to treat urethral stricture by the ventral sagittal urethrotomy approach without mobilizing the urethra. METHODS: Twelve patients with long or multiple strictures of the anterior urethra were treated by a dorsal free full-thickness preputial or buccal mucosa graft. The urethra was not separated from the corporal bodies and was opened in the midline over the stricture. The floor of the urethra was incised, and an elliptical raw area was created over the tunica on which a free full-thickness graft of preputial or buccal mucosa was secured. The urethra was retubularized in one stage. RESULTS: After a follow-up of 8 to 40 months, one recurrence developed and required dilation. CONCLUSIONS: The ventral sagittal urethrotomy approach for dorsal free graft urethroplasty is not only feasible and successful, but is easy to perform.
Dorsal buccal mucosal graft urethroplasty for anterior urethral stricture by Asopa technique. (Pisapati VL, Paturi S, Bethu S, Jada S, Chilumu R, Devraj R, Reddy B, Sriramoju V.) Eur Urol. 2009 Jul;56(1):201-5. Epub 2008 Jun 9.
BACKGROUND: Buccal mucosal graft (BMG) substitution urethroplasty has become popular in the management of intractable anterior urethral strictures with good results. Excellent long-term results have been reported by both dorsal and ventral onlay techniques. Asopa reported a successful technique for dorsal placement of BMG in long anterior urethral strictures through a ventral sagittal approach. OBJECTIVE: To evaluate prospectively the results and advantages of dorsal BMG urethroplasty for recurrent anterior urethral strictures by a ventral sagittal urethrotomy approach (Asopa technique). DESIGN, SETTING, AND PARTICIPANTS: From December 2002 to December 2007, a total of 58 men underwent dorsal BMG urethroplasty by a ventral sagittal urethrotomy approach for recurrent urethral strictures. Forty-five of these patients with a follow-up period of 12-60 mo were prospectively evaluated, and the results were analysed. INTERVENTION: The urethra was split twice at the site of the stricture both ventrally and dorsally without mobilising it from its bed, and the buccal mucosal graft was secured in the dorsal urethral defect. The urethra was then retubularised in one stage. RESULTS AND LIMITATIONS: The overall results were good (87%), with a mean follow-up period of 42 mo. Seven patients developed minor wound infection, and five patients developed fistulae. There were six recurrences (6:45, 13%) during the follow-up period of 12-60 mo. Two patients with a panurethral stricture and four with bulbar or penobulbar strictures developed recurrences and were managed by optical urethrotomy and self-dilatation. The medium-term results were as good as those reported with the dorsal urethrotomy approach. Long-term results from this and other series are awaited. More randomised trials and meta-analyses are needed to establish this technique as a procedure of choice in future. CONCLUSIONS: The ventral sagittal urethrotomy approach is easier to perform than the dorsal urethrotomy approach, has good results, and is especially useful in long anterior urethral strictures.
A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. (Mangera A, Patterson JM, Chapple CR.) Eur Urol. 2011 May;59(5):797-814. Epub 2011 Feb 24. Review.
CONTEXT: Reconstructive surgeons who perform urethroplasty have a variety of techniques in their armamentarium that may be used according to factors such as aetiology, stricture position, and length. No one technique is recommended. OBJECTIVE: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. EVIDENCE ACQUISITION: We performed an updated systematic review of the Medline literature from 1985 to date and classified the data according to the site of surgery and technique used. Data are also presented on the type of graft used and the follow-up methodology used by each centre. EVIDENCE SYNTHESIS: More than 2000 anterior urethroplasty procedures have been described in the literature. When considering the bulbar urethra there is no significant difference between the average success rates of the dorsal and the ventral onlay procedures, 88.4% and 88.8% at 42.2 and 34.4 mo in 934 and 563 patients, respectively. The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. When considering penile strictures, the success rate of the two-stage penile technique is significantly better than the one-stage penile technique, 90.5% versus 75.7% as calculated for 129 and 432 patients, respectively, although the follow-up of one-stage procedures was longer at 32.8 mo compared with 22.2 mo. CONCLUSIONS: There is no evidence in the literature of a difference between one-stage techniques for urethroplasty of the bulbar urethra. The two-stage technique has better reported outcomes than a one-stage approach for penile urethroplasty but has a shorter follow-up.
Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach (Asopa HS, Garg M, Singhal GG, Singh L, Asopa J, Nischal A.) Urology. 2001 Nov;58(5):657-9.
OBJECTIVES: To explore the feasibility of applying a dorsal free graft to treat urethral stricture by the ventral sagittal urethrotomy approach without mobilizing the urethra. METHODS: Twelve patients with long or multiple strictures of the anterior urethra were treated by a dorsal free full-thickness preputial or buccal mucosa graft. The urethra was not separated from the corporal bodies and was opened in the midline over the stricture. The floor of the urethra was incised, and an elliptical raw area was created over the tunica on which a free full-thickness graft of preputial or buccal mucosa was secured. The urethra was retubularized in one stage. RESULTS: After a follow-up of 8 to 40 months, one recurrence developed and required dilation. CONCLUSIONS: The ventral sagittal urethrotomy approach for dorsal free graft urethroplasty is not only feasible and successful, but is easy to perform.
Dorsal buccal mucosal graft urethroplasty for anterior urethral stricture by Asopa technique. (Pisapati VL, Paturi S, Bethu S, Jada S, Chilumu R, Devraj R, Reddy B, Sriramoju V.) Eur Urol. 2009 Jul;56(1):201-5. Epub 2008 Jun 9.
BACKGROUND: Buccal mucosal graft (BMG) substitution urethroplasty has become popular in the management of intractable anterior urethral strictures with good results. Excellent long-term results have been reported by both dorsal and ventral onlay techniques. Asopa reported a successful technique for dorsal placement of BMG in long anterior urethral strictures through a ventral sagittal approach. OBJECTIVE: To evaluate prospectively the results and advantages of dorsal BMG urethroplasty for recurrent anterior urethral strictures by a ventral sagittal urethrotomy approach (Asopa technique). DESIGN, SETTING, AND PARTICIPANTS: From December 2002 to December 2007, a total of 58 men underwent dorsal BMG urethroplasty by a ventral sagittal urethrotomy approach for recurrent urethral strictures. Forty-five of these patients with a follow-up period of 12-60 mo were prospectively evaluated, and the results were analysed. INTERVENTION: The urethra was split twice at the site of the stricture both ventrally and dorsally without mobilising it from its bed, and the buccal mucosal graft was secured in the dorsal urethral defect. The urethra was then retubularised in one stage. RESULTS AND LIMITATIONS: The overall results were good (87%), with a mean follow-up period of 42 mo. Seven patients developed minor wound infection, and five patients developed fistulae. There were six recurrences (6:45, 13%) during the follow-up period of 12-60 mo. Two patients with a panurethral stricture and four with bulbar or penobulbar strictures developed recurrences and were managed by optical urethrotomy and self-dilatation. The medium-term results were as good as those reported with the dorsal urethrotomy approach. Long-term results from this and other series are awaited. More randomised trials and meta-analyses are needed to establish this technique as a procedure of choice in future. CONCLUSIONS: The ventral sagittal urethrotomy approach is easier to perform than the dorsal urethrotomy approach, has good results, and is especially useful in long anterior urethral strictures.
A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. (Mangera A, Patterson JM, Chapple CR.) Eur Urol. 2011 May;59(5):797-814. Epub 2011 Feb 24. Review.
CONTEXT: Reconstructive surgeons who perform urethroplasty have a variety of techniques in their armamentarium that may be used according to factors such as aetiology, stricture position, and length. No one technique is recommended. OBJECTIVE: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. EVIDENCE ACQUISITION: We performed an updated systematic review of the Medline literature from 1985 to date and classified the data according to the site of surgery and technique used. Data are also presented on the type of graft used and the follow-up methodology used by each centre. EVIDENCE SYNTHESIS: More than 2000 anterior urethroplasty procedures have been described in the literature. When considering the bulbar urethra there is no significant difference between the average success rates of the dorsal and the ventral onlay procedures, 88.4% and 88.8% at 42.2 and 34.4 mo in 934 and 563 patients, respectively. The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. When considering penile strictures, the success rate of the two-stage penile technique is significantly better than the one-stage penile technique, 90.5% versus 75.7% as calculated for 129 and 432 patients, respectively, although the follow-up of one-stage procedures was longer at 32.8 mo compared with 22.2 mo. CONCLUSIONS: There is no evidence in the literature of a difference between one-stage techniques for urethroplasty of the bulbar urethra. The two-stage technique has better reported outcomes than a one-stage approach for penile urethroplasty but has a shorter follow-up.
Uretroplastica bulbare in tempo unico con innesto DORSALE di prepuzio
TECNICA: Incisione perineale ad Y rovesciata. Isolamento dell’uretra bulbare distale senza la sezione del centro tendineo del perineo. Apertura mediana ventrale dell’uretra, lungo il tratto stenotico [foto A1, A2]. Incisione mediana del piatto uretrale stenotico e lateralizzazione delle due bande di spongiosa [foto A3, A4]. Asportazione parziale del tessuto cicatriziale uretrale a livello della stenosi. Si confeziona uretroplastica di ampliamento dorsale (sec. Asopa) con innesto di cute prepuziale (prelevata dalla faccia dorsale del pene o tramite semicirconcisione o circoncisione) [foto A11]. Spongioplastica mediante sutura continua. Drenaggio. Parete a strati. Si consiglia Catetere Foley 18 Fr (siliconato e scanalato) per 21 giorni (sempre collegato al sacchetto della raccolta urine). Medicazione compressiva.
TEMPO DI ESECUZIONE: Circa 1,5h
TERAPIA: terapia antibiotica mirata in caso di urinocoltura positiva; antibioticoprofilassi con cefalosporina di III generazione in caso di uricocoltura negativa.
GESTIONE PAZIENTE: il paziente deve rimanere a letto per 2 giorni con ghiaccio sul perineo. Ghiaccio sulla guancia per 1 giorno. Dimissioni in 3° giornata postoperatoria.
MEDICAZIONI: La ferita perineale può essere pulita con acqua. Tra catetere e meato escono delle secrezioni-incrostazioni che vanno pulite più volte al giorno. Si consiglia di utilizzare acqua o soluzione fisiologica su una garza per pulire il catetere.
URETROCISTOGRAFIA MINZIONALE: Importante effettuare l’uretrocistografia minzionale di controllo, a 21 giorni dall’intervento chirurgico,per verificare se ci sono fistole.
QUANDO IMPIEGARE QUESTO TIPO DI URETROPLASTICA:Si può fare per una stenosi bulbare corta (< 2cm) o lunga (> 2cm), ma solo se la stenosi non è obliterativa. Quando si apre l’uretra, se il piatto uretrale è molto compromesso dorsalmente, viene parzialmente asportato e sostituito con il prepuzio. Questa scelta del graft può essere fatta ogni qual volta il prepuzio sia sano e ben rappresentato. Può essere indicata nei casi di ipospadia fallita (pazienti plurioperati per ipospadia) e nella ipospadia vergine. Sconsigliata, invece, nei casi di lichen sclerosus dell’uretra e dei genitali.
COMPLICANZE: sanguinamento <1%, infezione <2%. Fistola 4%
PERCENTUALE DI SUCCESSO CENTRO URETRA AREZZO: Casistica aggiornata al 30/06/2015. Effettuate 37 uretroplastiche bulbari in tempo unico solo con innesto di prepuzio. Percentuale di successo 91.2%.
CENTRO URETRA IN ITALIA: èpossibile effetuare una Visita con il Dr. Palminteri o la Dr.ssa Berdondini presso una delle principali sedi: Arezzo, Torino, Milano, Modena, Roma, Napoli, Reggio Calabria, Bari, Brindisi, Palermo, Catania, Messina, Trapani.
APPROFONDIMENTI:
Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. (Asopa HS, Garg M, Singhal GG, Singh L, Asopa J, Nischal A.) Urology. 2001 Nov;58(5):657-9.
OBJECTIVES: To explore the feasibility of applying a dorsal free graft to treat urethral stricture by the ventral sagittal urethrotomy approach without mobilizing the urethra. METHODS: Twelve patients with long or multiple strictures of the anterior urethra were treated by a dorsal free full-thickness preputial or buccal mucosa graft. The urethra was not separated from the corporal bodies and was opened in the midline over the stricture. The floor of the urethra was incised, and an elliptical raw area was created over the tunica on which a free full-thickness graft of preputial or buccal mucosa was secured. The urethra was retubularized in one stage. RESULTS: After a follow-up of 8 to 40 months, one recurrence developed and required dilation. CONCLUSIONS: The ventral sagittal urethrotomy approach for dorsal free graft urethroplasty is not only feasible and successful, but is easy to perform.
Dorsal buccal mucosal graft urethroplasty for anterior urethral stricture by Asopa technique. (Pisapati VL, Paturi S, Bethu S, Jada S, Chilumu R, Devraj R, Reddy B, Sriramoju V.) Eur Urol. 2009 Jul;56(1):201-5. Epub 2008 Jun 9.
BACKGROUND: Buccal mucosal graft (BMG) substitution urethroplasty has become popular in the management of intractable anterior urethral strictures with good results. Excellent long-term results have been reported by both dorsal and ventral onlay techniques. Asopa reported a successful technique for dorsal placement of BMG in long anterior urethral strictures through a ventral sagittal approach. OBJECTIVE: To evaluate prospectively the results and advantages of dorsal BMG urethroplasty for recurrent anterior urethral strictures by a ventral sagittal urethrotomy approach (Asopa technique). DESIGN, SETTING, AND PARTICIPANTS: From December 2002 to December 2007, a total of 58 men underwent dorsal BMG urethroplasty by a ventral sagittal urethrotomy approach for recurrent urethral strictures. Forty-five of these patients with a follow-up period of 12-60 mo were prospectively evaluated, and the results were analysed. INTERVENTION: The urethra was split twice at the site of the stricture both ventrally and dorsally without mobilising it from its bed, and the buccal mucosal graft was secured in the dorsal urethral defect. The urethra was then retubularised in one stage. RESULTS AND LIMITATIONS: The overall results were good (87%), with a mean follow-up period of 42 mo. Seven patients developed minor wound infection, and five patients developed fistulae. There were six recurrences (6:45, 13%) during the follow-up period of 12-60 mo. Two patients with a panurethral stricture and four with bulbar or penobulbar strictures developed recurrences and were managed by optical urethrotomy and self-dilatation. The medium-term results were as good as those reported with the dorsal urethrotomy approach. Long-term results from this and other series are awaited. More randomised trials and meta-analyses are needed to establish this technique as a procedure of choice in future. CONCLUSIONS: The ventral sagittal urethrotomy approach is easier to perform than the dorsal urethrotomy approach, has good results, and is especially useful in long anterior urethral strictures.
A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. (Mangera A, Patterson JM, Chapple CR.) Eur Urol. 2011 May;59(5):797-814. Epub 2011 Feb 24. Review.
CONTEXT: Reconstructive surgeons who perform urethroplasty have a variety of techniques in their armamentarium that may be used according to factors such as aetiology, stricture position, and length. No one technique is recommended. OBJECTIVE: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. EVIDENCE ACQUISITION: We performed an updated systematic review of the Medline literature from 1985 to date and classified the data according to the site of surgery and technique used. Data are also presented on the type of graft used and the follow-up methodology used by each centre. EVIDENCE SYNTHESIS: More than 2000 anterior urethroplasty procedures have been described in the literature. When considering the bulbar urethra there is no significant difference between the average success rates of the dorsal and the ventral onlay procedures, 88.4% and 88.8% at 42.2 and 34.4 mo in 934 and 563 patients, respectively. The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. When considering penile strictures, the success rate of the two-stage penile technique is significantly better than the one-stage penile technique, 90.5% versus 75.7% as calculated for 129 and 432 patients, respectively, although the follow-up of one-stage procedures was longer at 32.8 mo compared with 22.2 mo. CONCLUSIONS: There is no evidence in the literature of a difference between one-stage techniques for urethroplasty of the bulbar urethra. The two-stage technique has better reported outcomes than a one-stage approach for penile urethroplasty but has a shorter follow-up.
Uretroplastica bulbare in tempo unico con innesto DORSALE + VENTRALE di mucosa buccale
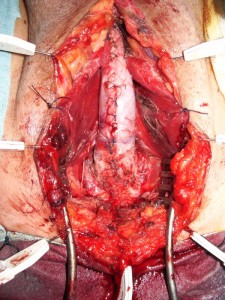
TECNICA: Incisione perineale ad Y rovesciata. Isolamento dell’uretra bulbare distale senza la sezione del centro tendineo del perineo. Apertura mediana ventrale dell’uretra, lungo il tratto stenotico [foto DV1,DV2]. Incisione mediana del piatto uretrale stenotico e lateralizzazione delle due bande di spongiosa [foto DV3, DV4]. Asportazione parziale del tessuto cicatriziale uretrale a livello della stenosi. Si confeziona uretroplastica di ampliamento dorsale ed ampliamento ventrale (sec. Palminteri), con innesto di mucosa buccale [foto DV5, DV6, DV7, DV9]. Il prelievo di mucosa buccale può essere unico e diviso in due parti [foto DV8] oppure, se non è sufficiente, può essere effettuato un prelievo da entrambe le guance. Spongioplastica mediante sutura continua [foto DV10]. Drenaggio. Parete a strati. Si consiglia Catetere Foley 18 Fr (siliconato e scanalato) per 21 giorni (sempre collegato al sacchetto della raccolta urine). Medicazione compressiva.
TEMPO DI ESECUZIONE: Circa 1,5h
TERAPIA: terapia antibiotica mirata in caso di urinocoltura positiva; antibioticoprofilassi con cefalosporina di III generazione in caso di uricocoltura negativa.
GESTIONE PAZIENTE: il paziente deve rimanere a letto per 2 giorni con ghiaccio sul perineo. Ghiaccio sulla guancia per 1 giorno. Dimissioni in 3° giornata postoperatoria.
MEDICAZIONI: La ferita perineale può essere pulita con acqua. Tra catetere e meato escono delle secrezioni-incrostazioni che vanno pulite più volte al giorno. Si consiglia di utilizzare acqua o soluzione fisiologica su una garza per pulire il catetere.
URETROCISTOGRAFIA MINZIONALE: Importante effettuare l’uretrocistografia minzionale di controllo, a 21 giorni dall’intervento chirurgico,per verificare se ci sono fistole. La percentuale di fistola uretrale insorta dopo uretroplastica bulbare, effettuate nel nostro Centro, è il 5%. Tutte le fistole uretrali sono state risolte mediante il posizionamento di catetere uretrale per ulteriori 10 o 15 o 20 giorni, a seconda dell’entità della fistola.
QUANDO IMPIEGARE QUESTO TIPO DI URETROPLASTICA:stenosi bulbare corta (< 2cm) o lunga (> 2cm), ma solo se la stenosi non è obliterativa. Questo tipo di uretroplastica è utile nelle stenosi molto serrate, in cui un solo apliamento dorsale o ventrale, non sarebbe sufficiente a creare un’uretra di calibro adeguato. Può essere indicata nei casi di lichen sclerosus dell’uretra e dei genitali, nonchè nei casi di ipospadia fallita (pazienti plurioperati per ipospadia) e nella ipospadia vergine.
COMPLICANZE: sanguinamento <1%, infezione <2%. Fistola 3%
PERCENTUALE DI SUCCESSO CENTRO URETRA AREZZO: Casistica aggiornata al 30/06/2015. Effettuate 197 uretroplastiche bulbari in tempo unico con mucosa buccale. Percentuale di successo 92.4%.
CENTRO URETRA IN ITALIA: èpossibile effetuare una Visita con il Dr. Palminteri o la Dr.ssa Berdondini presso una delle principali sedi: Arezzo, Torino, Milano, Modena, Roma, Napoli, Reggio Calabria, Bari, Brindisi, Palermo, Catania, Messina, Trapani.
APPROFONDIMENTI
Combined dorsal plus ventral double buccal mucosa graft in bulbar urethral reconstruction. (Palminteri E, Manzoni G, Berdondini E, Di Fiore F, Testa G, Poluzzi M, Molon A.) Eur Urol. 2008 Jan;53(1):81-9. Epub 2007 Jun
OBJECTIVES: We describe a technique for bulbar urethral reconstruction using a combined dorsal plus ventral double buccal mucosa graft (BMG). METHODS: From March 2002 to June 2006, 48 men, mean age 35 yr, with bulbar strictures underwent patch urethroplasty using a dorsal plus a ventral double BMG. Average stricture length was 3.65 cm (range: 2-10 cm). The stenotic urethral segment was opened along its ventral surface; the exposed dorsal urethra was incised in the midline to create an elliptical area over the tunica albuginea where the dorsal inlay BMG was placed and quilted to the corpora to augment dorsally the urethral plate. Subsequently, the ventral onlay BMG was sutured to the urethral lateral margins to complete the augmented urethroplasty. Finally, the spongiosum was closed over the graft. Successful reconstruction was defined as normal voiding without the need for any postoperative procedure including dilation. RESULTS: Mean follow-up was 22 mo (range: 13-59 mo). At the catheter removal 3 wk after surgery, in three patients the voiding cystourethrography showed a fistula, which recovered after a prolonged catheterization. Of 48 cases, 43 (89.6%) were successful and 5 (10.4%) failures with recurrence of the stricture; 4 were treated with internal urethrotomy and 1 with a temporary perineal urethrostomy. CONCLUSIONS: Preliminary results with a combined double BMG urethroplasty for severe bulbar stricture are encouraging. The double dorsal and ventral graft may provide a simple and reliable solution to achieve an adequate urethral lumen in selected patients.
Two-sided bulbar urethroplasty using dorsal plus ventral oral graft: urinary and sexual outcomes of a new technique. (Palminteri E, Berdondini E, Shokeir AA, Iannotta L, Gentile V, Sciarra A.) J Urol. 2011 May;185(5):1766-71. Epub 2011 Mar 21.
PURPOSE: Repair of bulbar strictures using anastomotic techniques may cause sexual complications, while 1-side graft urethroplasties may not be sufficient to provide an adequate lumen in narrow strictures. We evaluated the urinary and sexual results of a 2-sided dorsal plus ventral graft urethroplasty by preserving the narrow urethral plate in tight strictures. MATERIALS AND METHODS: Between 2002 and 2010, 105 men with bulbar strictures underwent dorsal plus ventral graft urethroplasty. The results are reported in a homogeneous group of 73 of 105 cases in which buccal mucosa was used as a graft with findings after 1 year or more of followup. The urethra was opened ventrally, and the exposed dorsal urethra was incised in the midline to create a raw area over the tunica albuginea where the first graft was placed dorsal-inlay. Thereafter the urethra was augmented by the ventral-onlay second graft and the spongiosum was closed over itself. Successful urethral reconstruction was defined as normal voiding without the need for any postoperative procedure. Postoperative sexual dysfunction was investigated using a validated questionnaire. RESULTS: Mean followup was 48.9 months and mean stricture length was 3.3 cm. Of these 73 cases 64 (88%) were successful and 9 (12%) were treatment failures with re-stricture. Furthermore, of 49 of 73 cases who were preoperatively sexually active, none reported postoperative erectile impairment and all were satisfied with their sexual life. CONCLUSIONS: In cases of tight bulbar stricture the dorsal plus ventral buccal mucosa graft provides adequate urethral augmentation by preserving the urethral plate and avoiding postoperative sexual complications.
A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. (Mangera A, Patterson JM, Chapple CR.) Eur Urol. 2011 May;59(5):797-814. Epub 2011 Feb 24. Review.
CONTEXT: Reconstructive surgeons who perform urethroplasty have a variety of techniques in their armamentarium that may be used according to factors such as aetiology, stricture position, and length. No one technique is recommended. OBJECTIVE: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. EVIDENCE ACQUISITION: We performed an updated systematic review of the Medline literature from 1985 to date and classified the data according to the site of surgery and technique used. Data are also presented on the type of graft used and the follow-up methodology used by each centre. EVIDENCE SYNTHESIS: More than 2000 anterior urethroplasty procedures have been described in the literature. When considering the bulbar urethra there is no significant difference between the average success rates of the dorsal and the ventral onlay procedures, 88.4% and 88.8% at 42.2 and 34.4 mo in 934 and 563 patients, respectively. The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. When considering penile strictures, the success rate of the two-stage penile technique is significantly better than the one-stage penile technique, 90.5% versus 75.7% as calculated for 129 and 432 patients, respectively, although the follow-up of one-stage procedures was longer at 32.8 mo compared with 22.2 mo. CONCLUSIONS: There is no evidence in the literature of a difference between one-stage techniques for urethroplasty of the bulbar urethra. The two-stage technique has better reported outcomes than a one-stage approach for penile urethroplasty but has a shorter follow-up.
Uretroplastica bulbare in tempo unico con innesto DORSALE + VENTRALE di mucosa buccale e prepuzio
TECNICA: Incisione perineale ad Y rovesciata. Isolamento dell’uretra bulbare distale senza la sezione del centro tendineo del perineo. Apertura mediana ventrale dell’uretra, lungo il tratto stenotico [foto DV1, DV15]. Incisione mediana del piatto uretrale stenotico e lateralizzazione delle due bande di spongiosa [foto DV4]. Asportazione parziale del tessuto cicatriziale uretrale a livello della stenosi. Si confeziona uretroplastica di ampliamento dorsale ed ampliamento ventrale (sec. Palminteri), con innesto dorsdale di cute prepuziale (prelevata dalla faccia dorsale del pene) [foto 16 ] ed innesto ventrale di mucosa buccale [foto DV17, DV18, DV19 ]. Spongioplastica mediante sutura continua [foto DV10]. Drenaggio. Parete a strati. Si consiglia Catetere Foley 18 Fr (siliconato e scanalato) per 21 giorni (sempre collegato al sacchetto della raccolta urine).
TEMPO DI ESECUZIONE: Circa 1,5h
TERAPIA: terapia antibiotica mirata in caso di urinocoltura positiva; antibioticoprofilassi con cefalosporina di III generazione in caso di uricocoltura negativa.
GESTIONE PAZIENTE: il paziente deve rimanere a letto per 2 giorni con ghiaccio sul perineo. Ghiaccio sulla guancia dove è stato fatto il prelievo di mucosa buccale per 1 giorno. Dimissioni in 3° giornata postoperatoria.
MEDICAZIONI: La ferita perineale può essere pulita con acqua. Tra catetere e meato escono delle secrezioni-incrostazioni che vanno pulite più volte al giorno. Si consiglia di utilizzare acqua o soluzione fisiologica su una garza per pulire il catetere.
URETROCISTOGRAFIA MINZIONALE: Importante effettuare l’uretrocistografia minzionale di controllo, a 21 giorni dall’intervento chirurgico,per verificare se ci sono fistole. La percentuale di fistola uretrale insorta dopo uretroplastica bulbare, effettuate nel nostro Centro, è il 5%. Tutte le fistole uretrali sono state risolte mediante il posizionamento di catetere uretrale per ulteriori 10 o 15 o 20 giorni, a seconda dell’entità della fistola.
QUANDO IMPIEGARE QUESTO TIPO DI URETROPLASTICA:Si può fare per una stenosi bulbare corta (< 2cm) o lunga (> 2cm), ma solo se la stenosi non è obliterativa. Questo tipo di uretroplastica è utile nelle stenosi molto serrate, in cui un sono apliamento dorsale o ventrale, non sarebbe sufficiente a creare un’uretra di calibro adeguato. Se non è sufficiente un prelievo di mucosa buccale, per effettuare un ampiamento adeguato del lume uretrale, si può utilizzare un innesto dorsale di prepuzio ed un innesto ventrale di mucosa buccale. Può essere indicata nei casi di ipospadia fallita (pazienti plurioperati per ipospadia) e nella ipospadia vergine. Sconsigliata, invece, nei casi di lichen sclerosus dell’uretra e dei genitali.
COMPLICANZE: sanguinamento<1%, infezione <2%. Fistola 3%
PERCENTUALE DI SUCCESSO CENTRO URETRA AREZZO: Casistica aggiornata al 30/06/2015. Effettuate 35 uretroplastiche bulbari in tempo unico con prepuzio e/o mucosa buccale. Percentuale di successo 94.6%.
CENTRO URETRA IN ITALIA: è possibile effetuare una Visita con il Dr. Palminteri o la Dr.ssa Berdondini presso una delle principali sedi: Arezzo, Torino, Milano, Modena, Roma, Napoli, Reggio Calabria, Bari, Brindisi, Palermo, Catania, Messina, Trapani.
APPROFONDIMENTI
Combined dorsal plus ventral double buccal mucosa graft in bulbar urethral reconstruction. (Palminteri E, Manzoni G, Berdondini E, Di Fiore F, Testa G, Poluzzi M, Molon A.) Eur Urol. 2008 Jan;53(1):81-9. Epub 2007 Jun 8
OBJECTIVES: We describe a technique for bulbar urethral reconstruction using a combined dorsal plus ventral double buccal mucosa graft (BMG). METHODS: From March 2002 to June 2006, 48 men, mean age 35 yr, with bulbar strictures underwent patch urethroplasty using a dorsal plus a ventral double BMG. Average stricture length was 3.65 cm (range: 2-10 cm). The stenotic urethral segment was opened along its ventral surface; the exposed dorsal urethra was incised in the midline to create an elliptical area over the tunica albuginea where the dorsal inlay BMG was placed and quilted to the corpora to augment dorsally the urethral plate. Subsequently, the ventral onlay BMG was sutured to the urethral lateral margins to complete the augmented urethroplasty. Finally, the spongiosum was closed over the graft. Successful reconstruction was defined as normal voiding without the need for any postoperative procedure including dilation. RESULTS: Mean follow-up was 22 mo (range: 13-59 mo). At the catheter removal 3 wk after surgery, in three patients the voiding cystourethrography showed a fistula, which recovered after a prolonged catheterization. Of 48 cases, 43 (89.6%) were successful and 5 (10.4%) failures with recurrence of the stricture; 4 were treated with internal urethrotomy and 1 with a temporary perineal urethrostomy. CONCLUSIONS: Preliminary results with a combined double BMG urethroplasty for severe bulbar stricture are encouraging. The double dorsal and ventral graft may provide a simple and reliable solution to achieve an adequate urethral lumen in selected patients.
Two-sided bulbar urethroplasty using dorsal plus ventral oral graft: urinary and sexual outcomes of a new technique. (Palminteri E, Berdondini E, Shokeir AA, Iannotta L, Gentile V, Sciarra A.) J Urol. 2011 May;185(5):1766-71. Epub 2011 Mar 21.
PURPOSE: Repair of bulbar strictures using anastomotic techniques may cause sexual complications, while 1-side graft urethroplasties may not be sufficient to provide an adequate lumen in narrow strictures. We evaluated the urinary and sexual results of a 2-sided dorsal plus ventral graft urethroplasty by preserving the narrow urethral plate in tight strictures. MATERIALS AND METHODS: Between 2002 and 2010, 105 men with bulbar strictures underwent dorsal plus ventral graft urethroplasty. The results are reported in a homogeneous group of 73 of 105 cases in which buccal mucosa was used as a graft with findings after 1 year or more of followup. The urethra was opened ventrally, and the exposed dorsal urethra was incised in the midline to create a raw area over the tunica albuginea where the first graft was placed dorsal-inlay. Thereafter the urethra was augmented by the ventral-onlay second graft and the spongiosum was closed over itself. Successful urethral reconstruction was defined as normal voiding without the need for any postoperative procedure. Postoperative sexual dysfunction was investigated using a validated questionnaire. RESULTS: Mean followup was 48.9 months and mean stricture length was 3.3 cm. Of these 73 cases 64 (88%) were successful and 9 (12%) were treatment failures with re-stricture. Furthermore, of 49 of 73 cases who were preoperatively sexually active, none reported postoperative erectile impairment and all were satisfied with their sexual life. CONCLUSIONS: In cases of tight bulbar stricture the dorsal plus ventral buccal mucosa graft provides adequate urethral augmentation by preserving the urethral plate and avoiding postoperative sexual complications.
A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. (Mangera A, Patterson JM, Chapple CR.) Eur Urol. 2011 May;59(5):797-814. Epub 2011 Feb 24. Review.
CONTEXT: Reconstructive surgeons who perform urethroplasty have a variety of techniques in their armamentarium that may be used according to factors such as aetiology, stricture position, and length. No one technique is recommended. OBJECTIVE: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. EVIDENCE ACQUISITION: We performed an updated systematic review of the Medline literature from 1985 to date and classified the data according to the site of surgery and technique used. Data are also presented on the type of graft used and the follow-up methodology used by each centre. EVIDENCE SYNTHESIS: More than 2000 anterior urethroplasty procedures have been described in the literature. When considering the bulbar urethra there is no significant difference between the average success rates of the dorsal and the ventral onlay procedures, 88.4% and 88.8% at 42.2 and 34.4 mo in 934 and 563 patients, respectively. The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. When considering penile strictures, the success rate of the two-stage penile technique is significantly better than the one-stage penile technique, 90.5% versus 75.7% as calculated for 129 and 432 patients, respectively, although the follow-up of one-stage procedures was longer at 32.8 mo compared with 22.2 mo. CONCLUSIONS: There is no evidence in the literature of a difference between one-stage techniques for urethroplasty of the bulbar urethra. The two-stage technique has better reported outcomes than a one-stage approach for penile urethroplasty but has a shorter follow-up.
Uretroplastica bulbare in tempo unico con innesto DORSALE + VENTRALE di mucosa buccale e prepuzio
TECNICA: Incisione perineale ad Y rovesciata. Isolamento dell’uretra bulbare distale senza la sezione del centro tendineo del perineo. Apertura mediana ventrale dell’uretra, lungo il tratto stenotico [foto DV1,DV15]. Incisione mediana del piatto uretrale stenotico e lateralizzazione delle due bande di spongiosa [foto DV4]. Asportazione parziale del tessuto cicatriziale uretrale a livello della stenosi. Si confeziona uretroplastica di ampliamento dorsale ed ampliamento ventrale (sec. Palminteri), con innesto dorsdale di cute prepuziale (prelevata dalla faccia dorsale del pene) [foto 16 ] ed innesto ventrale di mucosa buccale [foto DV17, DV18, DV19 ]. Spongioplastica mediante sutura continua [foto DV10]. Drenaggio. Parete a strati. Si consiglia Catetere Foley 18 Fr (siliconato e scanalato) per 21 giorni (sempre collegato al sacchetto della raccolta urine).
TEMPO DI ESECUZIONE: Circa 1,5h
TERAPIA: terapia antibiotica mirata in caso di urinocoltura positiva; antibioticoprofilassi con cefalosporina di III generazione in caso di uricocoltura negativa.
GESTIONE PAZIENTE: il paziente deve rimanere a letto per 2 giorni con ghiaccio sul perineo. Ghiaccio sulla guancia dove è stato fatto il prelievo di mucosa buccale per 1 giorno. Dimissioni in 3° giornata postoperatoria.
MEDICAZIONI: La ferita perineale può essere pulita con acqua. Tra catetere e meato escono delle secrezioni-incrostazioni che vanno pulite più volte al giorno. Si consiglia di utilizzare acqua o soluzione fisiologica su una garza per pulire il catetere.
URETROCISTOGRAFIA MINZIONALE: Importante effettuare l’uretrocistografia minzionale di controllo, a 21 giorni dall’intervento chirurgico,per verificare se ci sono fistole. La percentuale di fistola uretrale insorta dopo uretroplastica bulbare, effettuate nel nostro Centro, è il 5%. Tutte le fistole uretrali sono state risolte mediante il posizionamento di catetere uretrale per ulteriori 10 o 15 o 20 giorni, a seconda dell’entità della fistola.
QUANDO IMPIEGARE QUESTO TIPO DI URETROPLASTICA:Si può fare per una stenosi bulbare corta (< 2cm) o lunga (> 2cm), ma solo se la stenosi non è obliterativa. Questo tipo di uretroplastica è utile nelle stenosi molto serrate, in cui un sono apliamento dorsale o ventrale, non sarebbe sufficiente a creare un’uretra di calibro adeguato. Se non è sufficiente un prelievo di mucosa buccale, per effettuare un ampiamento adeguato del lume uretrale, si può utilizzare un innesto dorsale di prepuzio ed un innesto ventrale di mucosa buccale. Può essere indicata nei casi di ipospadia fallita (pazienti plurioperati per ipospadia) e nella ipospadia vergine. Sconsigliata, invece, nei casi di lichen sclerosus dell’uretra e dei genitali
COMPLICANZE: sanguinamento<1%, infezione <2%. Fistola 3%
PERCENTUALE DI SUCCESSO CENTRO URETRA AREZZO: Casistica aggiornata al 30/06/2015. Effettuate 35 uretroplastiche bulbari in tempo unico con prepuzio e/o mucosa buccale. Percentuale di successo 94.6%.
CENTRO URETRA IN ITALIA: è possibile effetuare una Visita con il Dr. Palminteri o la Dr.ssa Berdondini presso una delle principali sedi: Arezzo, Torino, Milano, Modena, Roma, Napoli, Reggio Calabria, Bari, Brindisi, Palermo, Catania, Messina, Trapani.
.